Learn From the Dental Industry's TOP LEADERS!
Sit Chairside withDr. Dennis WellsCreator ofDURAthin® Prepless Veneers- OR -
|
Finding and Treating Sleep Apnea in Your PracticePart 1 - Sleep apnea overview
Instructors:
Dr. Kent Smith reviews sleep apnea and the key terms that are associated with sleep apnea.
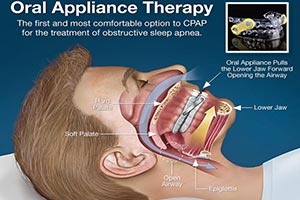
I am Dr. Kent Smith and we're here at 21st Century Dental my practice where we do a lot of treating sleep apneic from the practice. I would say it's about 35% to 40% of my practice and it's growing. We will be doing that, probably the majority of the practice will be involving treating these snores and sleep apneic with in the next year or so. So, it's become a huge part of practice. Ad we're going to go through today some of the things that we do in our practice to treat these, to screen them, to find out just who our patients that might have the sleep breathing disorders and then the step by step procedures of going through that. You know we're so used to looking at the oral cavity that we'd often times miss out on some things that we really should be seeing as a dentist. So let's get started in talking about what we do. But first I want to show you what sleep apneic looks like when he's asleep. Now this is a guy who is on his side. It's not even a worst case scenario. If he was on his back it would be worst. But he has realized through the years that sleeping on his side is the only way that he can get through tonight. So as you can see here he's occluded. He's trying to breath but he can't draw any air. He's trying. He's trying. This is called obstructive sleep apnea. There's an obstruction so he can't draw that breath. At some point he wakes up just enough like he did there. He moves his jaw a little bit. He draws the breath of air and then he falls back to sleep and then he's occluded again. And this goes on night after night after night. It has lots of wear and tear on the heart as you can imagine. Create all kinds of fatigue because he's waking up consistently called microarousals. So this guy is going to be very very fatigue and it's a wear and tear on his whole system. Every organ in the body is affected by this lack of oxygen that he gets. So let's go over a few key terms that I think is important for you to understand especially as we go through this presentation. I want you to understand a few of the things that we mentioned but OSA that guy right there had obstructive sleep apnea. There's essential two different types. There's obstructive sleep apnea and then there is central sleep apnea. In central sleep apnea, they aren't trying to take a breath. It's where the brain's respiratory center just says don't bother to breath. That's central sleep apnea. Now one way we measure the severity of the apnea is through the apnea hypopnea index or the respiratory disturbance index. So when I mention the AHI or RDI that's what I'm talking about. And essentially it just means how many times does this guy stop breathing per hour for at least 10 seconds at a time. If he stops breathing less than 5x an hour, we say he doesn't have sleep apnea. If he stops breathing between 5 and 15, he has mild. Between 15 and 30 he has moderate. And if he has more than 30x per hour where he stops breathing for 10 seconds or more, that is considered severe sleep apnea. And that's the way it's graded. It will be graded that way when we file medical insurance. Insurance will not cover unless the condition is severe enough. So that's one way that we judge this. We aren't the diagnosticians however. The sleep physician does the diagnosis. We get this from the physician and then we use this information to file medical insurance for our patients. And then finally we look at desaturation. Desaturation, those of you that treat patients in your practice with sedation, you realize that you don't want them to go below 90% saturation. And so the same thing during sleep, we don't want them to be saturate below that. So we're looking at that consistently with every study that we get we want to now how long they were under 90% saturation. And we like them to stay above that 90%. I'm going to show you a few of the patients that we had this week just to show you how prevalent it is. These are patients just coming through our practice. This is Ryan. He was a new patient in the hygiene department. He had a heart attack at 30, snores consistently. Unfortunately, the cardiologist and you'll find this many times, the cardiologists area really not well educated in sleep apnea. Never refer the patient for a sleep study so we did. We'll wait to see what happens but I have a feeling he's going to have severe sleep apnea. Heart attacks are one of the signs and symptoms that we see with this apneic patients. This is Gilbert. Gilbert came in actually a few weeks ago as a new patient. He had an AHI of 4.5 10 years ago. As you can see he didn't have sleep apnea cause it was less than 5. Eleven years later he did another study 37.8. He went from no apnea to severe apnea. As you get older, as you gained weight, those are the two things that increase your likelihood of developing sleep apnea. He's actually an engineer and you all have engineer patients but he said you know what those CPAP machine I can build a better CPAP. So he wanted the SomnoDent. We deliver it this week. This is Navid. Navid is a typical patient that flies all the time. We're in the Dallas area. We have Dallas Fort Worth airport 15 minutes from us. And so we have a lot of these patients that fly a lot. He uses a CPAP and he likes it. But you can't wear one of those on the plane and when you not asleep on the plane and you start snoring, the people around you don't appreciate that. So he decided that he wanted something just for travel. They also don't like taking them through the metal detector that's a big pain. And he owns this gold to cash stores and he said can I just give you some gold for this thing. We'll see. This is James. James had severe apnea back in 2009 but it wasn't affecting him enough evidently to seek treatment. He tried CPAP. He couldn't wear it. Three years later, his AHI has gone to 115, tremendous increase in sleep apnea. This guy every 30 seconds stops breathing for at least 10 seconds. He gained some weight and so gaining weight makes it worst. So we deliver SomnoDent this week. This is Bill. His wife sent him in for snoring, just snoring. And we did a home study on him and during the home study the AHI was 67. So remember more than 30 is severe. He's very severe and all his wife sent him in for was snoring. A lot of your snoring patients do not know they had sleep apnea. In fact, 90% are undiagnosed. So it is really your job as a dentist to get them diagnosed in your practice. The physicians don't have time. They have no time in their practice with manage care the way it is, all they have time for is to look at their chief complaint whether it's diabetes or ulcers or asthma. You know they're treating things like that and they don't have time to ask them about breathing and sleeping. So that in my opinion that makes the dentist the frontline and we are the caretakers of this type of a patient. This is Dana. This is a sad story. She said that she actually remembers in the living room her father snoring on the couch and he was snoring and snoring and he stopped snoring and then he slumped over and died. She said I don't want that to happen to me. We did a sleep study on her. It was 32.8 and we take impression for an appliance. We're preventing drivers from falling asleep at the wheel. We're getting spouses back together and that's huge. We have spouses that haven't slept together in 20 years because the wife, the bed partner of a snorer loses an hour and a half sleep every night, an hour and a half. So they get very irritated at the bed partner. You know we prevent a lot of marital problem in their sleeping. So I've had a lot of thank you from spouses coming back in and saying thank you so much. Shirley is sleeping with me again. It's so important. So there's very noble reason for doing it. But listen you all run a business and so making money out of this is not a bad thing. We average, because medical insurance is reimbursing for this, we average around $4,000 every time we treat one of these patients. The medical insurance is just sending us checks. I don't know if that should be the reason you treat these patients but it sure doesn't hurt because you're looking for ways to increase the income in your practice. This is what the home study looks like. We have quite a few of these home units at our practice because many patients will not go for a full polysomnogram at a sleep center. So these are home studies and they're pretty detailed. In 2008, Medicare therefore medical insurance companies out there made the statement their new protocol is home units can be used to diagnose sleep apnea. And so when that happened, a lot of these ambulatory or home unit manufacturers started improving their units. You can imagine many apneic that are out there, they wanted to have the best machine out there. So this keeps improving. They keep getting better. The technology keeps improving. This is what a Watch PAT looks like. A report from a Watch PAT and it gives us a full story of the patient. It shows that she has severe sleep apnea, that she desaturates. It shows her heart rate and what happened to the heart rate as she goes to the night and how apnea affects the hart. It shows different sleep architecture. How much REM deep sleep, light sleep, etc. the patient had. It talks about how bad their apnea was on their back, improve on their side. There's a lot of good data in this home units. Okay. Let's talk about the different types of sleep breathing disorders. You know about snoring. After you snore long enough before you develop sleep apnea, you can develop what we called upper airway resistance syndrome or UARS. That's when you have a fatigued snorer. They're sleepy but they still don't have sleep apnea because they wake up a bunch during the night not even knowing that they woke up. Then it develops into obstructive sleep apnea when they stop breathing at least 5X an hour for 10 seconds at a time. Central sleep apnea as I mentioned it's usually the older patients or some sick patients where the respiratory center just isn't sufficiently activated to tell the brain take a breath. The patient just takes a breath off and says I'm just not going to breath. We can't fix that with oral appliances. That's where you have to have a CPAP unit. Then there is mixed where you have a combination of central and obstructive sleep apnea and then complex when a patient goes into a sleep lab they are given a sleep CPAP machine and they originally have obstructive sleep apnea. They put the machine on and the body says oh I got this machine breathing for me, no need to breath. So they developed central sleep apnea after they had obstructive. So that's a complex situation and again that requires a specific type of CPAP machine.
|
 Submitting...
Submitting...


 FAGD/MAGD Credit Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement 7/31/2018 to 7/31/2021 Provider ID# 317928
FAGD/MAGD Credit Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement 7/31/2018 to 7/31/2021 Provider ID# 317928