Learn From the Dental Industry's TOP LEADERS!
Sit Chairside withDr. Dennis WellsCreator ofDURAthin® Prepless Veneers- OR -
|
Joint assessment and understanding joint soundsPart 1 - Risk assessment and management
Instructors:
Dr. Lee Ann Brady discusses how to achieve predictable success of TMD and reviews evaluation, diagnosis, treamtment options and creating patient awareness.
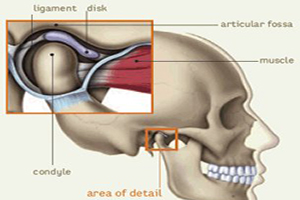
Hi, I'm Dr. Lee Ann Brady. Thank you for joining me here on HDiQ for a program today on joint diagnosis and understanding joint sounds. Just to lay the foundation for what we're going to go ahead and talk about. Really I wanted to share that I think about this as part of my process of risk assessment. And so for all of my patients in my office whether I'm talking about carries or I'm talking about joints, it really does start at the foundational level of thinking about risk management. The important piece with risk assessment is that then I do get to manage it. I get to figure out with the patient together what are the things we can do to ameliorate or eliminate the risk. How are we going to move forward so that over time they can keep their teeth as healthy, as comfortable, as functional and as esthetic as possible? And those same parameters apply when I think about joint diagnosis and doing a joint exam. And so what is the foundation as we think about having predictable success in our practices cause honestly that what it's all about. When I come into my office everyday what I want to know is that I have the peace of mind and my patients have the peace of mind that we're going to be able to predictably have them keep their teeth healthy and then any work we do together we can know predictably what those procedures will look like and what the outcomes will look like. So really for more me that predictability comes from following a process, a system that applies to everything that I do in my office. And so, predictability always starts with evaluation, with doing an exam, with understanding the present condition, and then taking that information and coming up with the diagnosis. And one of the things that I do believe in dentistry is that there is one diagnosis so that that's the core off, then how we come up with our treatment options. And one of the things I also believe is that for any diagnosis there can be a multitude of treatment options. And how we actually come up with what we're going to do together is a combination of the patient's circumstances and objectives and their interest as well as what the risk and benefits are of different opportunities for treatment that they have. So you'll notice on this list the last piece of that is patient awareness. Because a huge piece of predictability is knowing that we're partnering together. That they understand just like I understand what the risks are and what we're going to try to do to manage those things moving forward. So now especially let's start our conversation about joint diagnosis and understanding joint sounds. For me that starts with a history. Joints are an interesting thing in our practices. A lot of folks that I meet in dental practice and I was one of these folks for many years were a little daunted by patients that have joint sounds or come in complaining about joint pain. So really being able to feel confident at understanding what's going on and confident at treating it if you're going to choose to do that. Because being able to evaluate and diagnose a joint issue does not mean you'll necessarily going to choose to treat those in your office but you can make a decision of where our patient is safe to move forward with restorative dentistry or other types of treatment like orthodontics without having to treat what's going on with our joint. And who are the patients that need some kind of intervention around their joint prior to other therapy and who am I going to refer those patients to if I'm not going to treat them in my own office. So we start with a history and when we come to a joint evaluation, the history really gives us a large majority, I'd even say a lion's share of the information that we need. So really being able to put the puzzle together of what we learned during the exam starts with a thorough history. So what are the things that we want to know from a patient. As best as possible I really want to get them talking about what's going on with their joints. What they're experiencing now but also what they're also experiencing in the past. And I think about this as three when's. Because there are three pieces in that information about joint pain and joint sounds that are vital at unraveling the puzzles of what's going on today. One is is it happening now. So is the pain they're telling us about or is the sound present now? So that when they go ahead and they open and close their mouth now today in my office can they actually elicit those joint sounds and/or are they feeling that pain. That's a really important piece of the puzzle. Not only as it gives me clinical information but it's important to that patient awareness piece. So when we think about joint sound and we say someone had a pop or click in the past, but now that sounds has gone away. Immediately we're all thinking as dental professionals I wonder what happen because the situation has gone downhill. In contrast to that what a patient also think when a joint sounds go away. Exactly. They think it got better.So there's a piece of having that conversation and explaining what's going on that begins that process of awareness. The next when that I want to know about joint pain or joint sound is when during the day is it happening. So is the pain present all the time or only when they go to chew, only when they yawn or open wide. Is it only when they eat hard foods or is it anything that they chew? Is it present for the last two weeks or it's been six months? So those are important pieces. Same thing for joint sounds. Some patients will tell me that their joint pops sometimes. I want to get to the bottom of when is that. Is it first thing in the morning when you wake up? Is it only after you workout during the day and you're exercising. Is it after you spent two hours at your computer or is it every single time that the patient open and closes. I also want to know the when of when does it occur in jaw movement. Now that's a piece we're going to come to when we talk about joint diagnosis. Cause the patient can't unravel that.So two of the when's: when in time meaning the past or present and when during the course of the day are things that we can get most of our information during the patient history. We're going to answer the when in the movement of their mandible, those sounds are occurring. And that's a critical piece. So as we start our joint exam for me one of the very first pieces that I do is I want to just observe the patient's opening and closing stroke. So I will have the patient simply open and close several times for me. I'm actually eyeballing a place, their midline of their upper whether that be the center of their philtrum or if I can see their upper teeth, the midline of their upper central incisor and I eyeball a place on their lower, on their mandible. Same thing. It can be soft tissue on their lip or if you can see their incisor. And I want to just watch and track how they open and close. So is it nice and smooth and even in their mandible track straight up and down or do they halt, hesitate, have to stop or start and is there some deviation or change in direction? And I also want to know if they do change direction, are they changing on opening or on closing stroke or both? So I'm going to simply observe those and I have a place on my exam form where I'm going to keep track of that information. Honestly it looks like a little T like a cross bar and then we literally draw in red and green pencil. So we do the opening stroke in red and then we flip the pencil over and do the closing stroke in the other color. So we know always which was opening and which was closing. We document it. I typically will do this at the same time that I actually have my hands over the lateral poles of the condyle cause what I'm doing is I'm isolating the lateral poles for the next part of my exam, but I'm also palpating what we called palpable joint sounds. So, palps or clicks that I can feel under the tips of my finger. And if there is a palpable joint sound and I see a deviation on opening or closing I'll actually record the timing of those two things. So is the deviation coincident with when I feel that palp or that click. So that's important information when I look at those opening and closing strokes. Next is we think about our joint evaluation. I'm going to move into my palpations. Now a lot of this for me when I said I observed opening and closing; have my hands on the patient's face and now I'm going to do my palpations. I actually have a particular preference. I prefer to do the extra-oral part of the exam without gloves on. So as I said in my other video where I do a joint and muscle exam, that's up on HDiQ. I ask the patient's permission so I'll ask them since I'm going to be extra-oral. Would it be okay with you if I do this exam without gloves on if I watch my hands first? And I make a big deal of washing my hands in front of the patient. Actually patients are so intuitive. I just had a lady that saw this Friday of last week who I asked that of and she said, ìOh, absolutely. I'm guessing that you have a better feel in your fingers of what's going on if you don't have gloves on.î It's exactly why I do it. I don't want my perception, that tactile perception to be deadened by the latex or [0:09:18][inaudible]. So as I start my joint evaluation and my palpations, the first thing I'm going to palpate is the lateral pole of the condyle. So I'm going to isolate the lateral pole of the condyle with one finger and for all palpation it's pressing in. You want to have for a joint palpation about a pound of pressure as you're pressing in. So just enough to blanch your fingernail bed and then release. And now you're going to have feedback from the patient. So I always tell patients when I started joint palpation that really the most critical information is going to come from them giving me their feedback about what it feels as I do the exam. That pressure, the sensation of me pressing is totally normal. Anything beside just pressure is important for me to know whether it's a mild tenderness all the way up to an extreme pain. And I actually use a scale that's 1 to 10. I like having that ability to differentiate fine differences where mild, moderate and severe doesn't give me as much information. And I also always remember that the report the patient gives me is only relative to them. So one patient saying that a lateral pull palpation is a 3 and someone else saying it's a 6 doesn't mean that the person has 6 has more severe inflammation or is in more pain. Its patient's perception where those numbers are important is when I do something. So I make the patient an appliance. We put them on anti-inflammatory. We start to put them on a soft diet and then we do the pieces of the exam. If the numbers have lessen then I can draw a correlation between the therapy we applied and the resolution of their pain or their inflammation that was causing that. So we'll use that scale of numbers. For a lateral pole palpation again it's just fingers over the lateral poles. For me, you'll see I do that in the other view where we go through clinically the entire exam. I actually have the patient with their teeth just lightly touching, not clenching, press and release and I get the patient's feedback from that. So what am I doing in a lateral pole palpation? What I'm actually doing is I'm compressing the capsule on the outside of the temporal mandibular joint and the synovial membrane between my finger and the lateral pole of the condyle. So if a patient says yes. They have tenderness or discomfort there, what I know is that there's an inflammatory process that's present in that capsule or in the synovial membrane that's responsible for that discomfort. So at this point, sort of my clinical suspicion or my differential is going to be either capsulitis or synovitis. I don't know what's causing it. At this point I don't have enough information to say what I would do about it, but I do know there's inflammation either in the capsule or in the synovial membrane.The next part of my exam is going to be to palpate retrodiscal tissue or the posterior aspect of the temporomandibular joint. The restrodiscal tissues are the highly innovated, highly vascular tissues that are behind the head of the condyle in the temporomandibular joint. So as I'm palpating those I do want to be a little bit less pressure applied because it's very easy to get a false positive. For me the way I do this I simply have the patients open as wide as possible. I now have my finger so that I can press sort of in and forward against the posterior lateral aspect of the condyle and I'm actually compressing those retrodiscal tissues now against that posterior lateral aspect of the condyle. If I get a positive response with the retrodiscal palpation, what I know is that there's an inflammatory process in that retrodiscal tissue. Again I don't know what's causing it. I may be starting to formulate a thought process of what the treatment might be to resolve that. I can be thinking about things that could be impinging on the retrodiscal tissues. That's one of the things we'll unravel in the rest of the exam starting to put those puzzle pieces together. That's doing a retrodiscal tissue exam. |
 Submitting...
Submitting...

 FAGD/MAGD Credit Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement 7/31/2018 to 7/31/2021 Provider ID# 317928
FAGD/MAGD Credit Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement 7/31/2018 to 7/31/2021 Provider ID# 317928