Learn From the Dental Industry's TOP LEADERS!
Sit Chairside withDr. Dennis WellsCreator ofDURAthin® Prepless Veneers- OR -
|
Finding and Treating Sleep Apnea in Your PracticePart 4 - Treatment of sleep apnea
Instructors:
Dr. Smith reviews the three different options for treating sleep apnea.
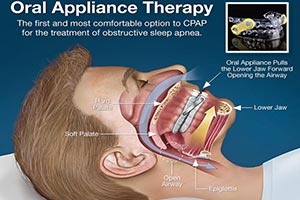
All right, let's talk about treatment. There are many ways to treat this but really just three basic ways. So when we have a consultation with the patient we talk about the three major ways CPAP, surgery, and oral appliances. Those are the three basic ways. You're going to hear all kinds of way on the internet and on TV you're going to find all kinds of ways to treat it with pillows and all kind of stuff. But the only three things that are really considered viable treatment options for patients by the American Academy of Seep Medicine, which is the group of sleep physicians, are CPAP, oral surgery and mandibular advancement devices. So we're really going to talk about mainly those three. But you will hear things like [0:27:53][inaudible] or lubricants and all kind of stuff that's out there. I will say that the American Academy of Sleep Medicine has come up with their new protocol a few years ago where they said there's enough research into oral appliances for mild and moderate the patient has the choice because it's just as effective on mild and moderate patient as CPAP. If neither CPAP or oral appliances will work, if the patient will not use either one then surgery. But there's not enough research behind surgery to put it into same category as oral appliances. So sleep physicians should be sending patients, once the patients become CPAP intolerant should be sending them to you, the dentist, to get treated with an oral appliance before surgery. This is what the CPAP looks like. It's called the pneumatic splint. You just crank up the pressure as high as you need to so that it blows past any obstruction that there is. That's one reason they come intolerant to it because the obstructions are such that you have to turn the pressure up really high. It's almost leaning your head up the car window, rolling down the window, leaning it out, opening your mouth as 65 miles an hour. It's not really easy. So the compliance rates for CPAP are much less than they are for oral appliances. That's why we see a lot of patient that are CPAP intolerant come to our practice for oral appliances. These are some of the design. There's all kinds of mask. They're trying to find something that works for the patient. Everybody got a different shaped face so it's really difficult sometimes to find the mask that fits and feels comfortable for the patient but they're doing all they can. Surgery. There's a bunch of surgeries or the U-Triple-P which is just a roto-rotter at the back of the throat. There's all kinds of [septoplasty]. There's coblation where you use energy and radio waves. You're decreasing the mass of the tongue for example or oral pharyngeal tissues. That's one of the newer techniques. It's called oblation so you don't have collateral damage. All kinds of surgery. We will not go into that too much because of you most wont' be doing those surgeries. This is what it might look like after you a U-Triple-P surgery. As you can see, it does clear out the back of the throat pretty well. They can be effective but it is a very painful procedure to go through. Not something I would submit a patient to until they haven't been able to use an oral appliance. Now there are different kinds of mandibular advancement devices that are out there. There might be a hundred out there now. I mean I don't know how many there are. They need to be FDA cleared for insurance to cover those. So make sure if you use an oral appliance to use for this that it is FDA cleared so that you can get your patient's medical insurance to reimburse them. I used a SomnoDent, the SUAD, the OASYS, the Tap, the Herbst, Moses and there's others that I use in my practice but SomnoDent is my favorite. But it doesn't work on everybody so you kind of have other appliances available to use. Just whatever appliances you choose make it your go to appliance. Make it your favorite and use it most of the time but realize one specific appliance does not work well for every patient. This is what the SomnoDent looks like. I like it for a few reasons mainly because the arches aren't connected. They can open and close. Many of my CPAP intolerant patients come to me because they're claustrophobic. If you put them in an appliance that keeps their mouth close that doesn't do well with their claustrophobia. So the SomnoDent or other appliances that don't keep the jaws together, it allows them to open and close, patients tend to adapt better to. So that's one reason I really like the SomnoDent. You can put a discluding element on it to open the vertical. This is the Tap 3 and it's a great appliance out there. The arches are together but it's easy to adjust the appliance because the patient slide the lower jaw forward, gets them into that hook and even the bed partner can reach forward and crank that thing forward if the partner is still snoring. So the Tap is a good appliance. It's one of my appliances that, ops sorry. The OASYS is another one. It's an excellent appliance as well. It uses nasal dilators to open the nasal pharynx a little bit. It also can be used on gagging patient because there's not maxillary component to it. So again it can be use as your go to appliance. It can be used as your appliance you use on everybody. This is the SUAD. It looks mean. There's a lot of metal here but it's really pretty comfortable. And from that patient that are going to break everything and you've got those huge masters and this big guy, this 400-lb guy that's going to break whatever you put in his mouth, I'm going to put him in a SUAD. This is the George Gauge bite registration. This is what we used on every patient to get their bite. You need to figure out at what point you want the bite set with the appliance when it comes back because these are titratable appliance. We will be adjusting the patients further forward or telling the patient to look for silence and lack of fatigue. But we have to start them at some point and this George Gauge allows us, it's kind of the industry standard out there. There are other techniques for getting a bite registration. This is the most common one. And we can set it for example at a 70% maximum protrusive. That's about where most patients can go and be comfortable starting out. And in our moderate to severe patients, you're going to need to get them out there. So we start them at a protruded position and then go from there. Very important that you follow up and if there's anything that you get from this entire presentation today, now we're going to be talking to a patient in a little bit to show you how we go through a patient in the consult and the interview and all the things that we look for in their sleep study and everything, but the most important thing is you follow this patient up. If a physician prescribes a medication for hypertension for example would he even bother taking the blood pressure afterwards or would he just let the patient go and not follow up. No. He always wants to know did the therapy do the job. And the only way to do that is to test afterwards. I can consider it a malpractice to put somebody in an appliance and not follow up and do a study with them afterwards. If you don't do that, you can create what we called silent apnea. Silent apnea is when they're no longer snoring. The patient thinks they're okay but they're still not breathing. The bed partner says they're not snoring. I can show you study after study that shows example of somebody who is not snoring, but they still have severe sleep apnea. So it is vital to follow them up. We follow them up with these ambulatory units. You can use a sleep study at a sleep center to follow them as well but many patients will not go back. They've already had an initial study to diagnose them at a sleep center and it was not a good experience. They don't want to go back. So what do you do? You can't get them to go to a followup study. You do your best but without home units you can't do it as well. So it's another reason why I suggest having these things they really allow you to do a good job following your patients up. So can sleep dentistry profitable. Medical instrument is paying for these things now. We're getting anywhere from a thousand dollars from Blue Cross, Blue Shield. All the way up to, I mean we get thousands more from other insurance companies. It can be very profitable. So if you're looking for another profit center in your practice, this can be it. So you're going to be saving lives and marriages. You're going to be keeping sleepy drivers off the road, etc. but if you can do that and make money that's not a bad thing. So I do teach full courses on this. You can go to sleepdallas.com to find out more. You can just be screening these patients and then sending them out to somebody for treatment. But if you want to really make this a significant part of your practice I would urge you to get started. Take a course. I'm not the only one that teach courses out there. There are many other courses. So feel free to contact me as well. I can give you any kind advice through email or over the phone if you like. So thank you for being with us today and I hope that you've gained enough knowledge to know where you want to go from here. |
 Submitting...
Submitting...


 FAGD/MAGD Credit Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement 7/31/2018 to 7/31/2021 Provider ID# 317928
FAGD/MAGD Credit Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement 7/31/2018 to 7/31/2021 Provider ID# 317928