Learn From the Dental Industry's TOP LEADERS!
Sit Chairside withDr. Dennis WellsCreator ofDURAthin® Prepless Veneers- OR -
|
Finding and Treating Sleep Apnea in Your PracticePart 5 - Patient consultation
Instructors:
Dr. Smith demonstrates how to verbalize the need for treatment to a patient.
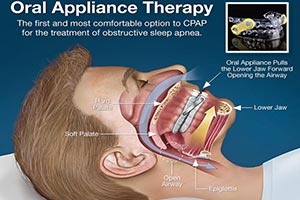
I usually have April come in. This is largely a delegated procedure. You know April will see the patient, my sleep assistant. And then she'll go over a lot of the things that I'm going to be doing with Kelly here today. But for purpose of this I'm just going to be doing it myself and just know that you can delegate most of this to a very able assistant. Now, April had a lot of training and you got to get an assistant to go through the courses and learn all of this so that they know how to talk to the patient. Not everybody will have an April but I've got my April so that's who does most of this for me. Well Kelly, welcome back. So I know that you came through our hygiene department and we were asking you about your sleep and that's when you said something about the CPAP machine that you were using and that wasn't your friend. No, love-hate relationship and I just can't handle the hose and all the connections. There's a lot to that. Yeah. You've got to change the filters and you've got the humidifier always, keep changing the water out and all that kind of stuff and it's not real sexy. And then I want to sleep on my stomach and that's like∑ Hard to sleep on your stomach. Yeah, that's true. So I will arrange to have a sleep study from your sleep physician. I got a few days ago and I've gone through it and look at some things. But I'm going to be going over some of these with you but I would like to know you know back in 2003, this is when you originally have the study, what was the original reason for the study? What got you in there? Why did you seek treatment? Well first of all, my husband told me that I was snoring really loud and then stopping. I would stop breathing throughout the night. He called me and I just keep going. I never stop. But he wanted me to go and see about it. Well I didn't do it so he went on and taped me. He taped you with the tape recorder. Back in 2003, we didn't have the cellphone where we had apps on there where we can actually record snoring. So he used a tape recorder. Yes. Okay. Impressive. So this recorded snoring and your breathing pauses. Yes. My breathing pauses so with that I went on and took action. And I also have problems with circulation. Okay. And I had problems with diabetes and just totally fatigued. So we end up going to see a doctor reference to my neuropathy I thought I had in my feet. Okay. And he kind of ruled out different things from that. The doctor did testing on my feet. He said there was nothing wrong. But I was exhausted. I didn't have the mental clarity. I was gaining weight. There was a lot of issues there. So he decided to send me to have a sleep study done. Okay. This says you had asthma; you had diabetes and some depression too. Yes. Is that related to the fatigue? Yes. Something very common that we see in patients, when look at our health histories we look for medications that our patients are taking. And one of the things that we look for are those related to depression. So any antidepressant that the patient is taking, anything that has to do with GERD, acid reflux if they're taking medications like that that's something that you should be looking at with your health history. I called it the nocturnal health history. Look at all the medications you're taking and try to relate it to way they're sleeping. So you had the study, then they gave you the CPAP machine. Yeah. I'm just curious did they tell you at that time, hey, Kelly you got an option. You got a CPAP machine and then we've got oral appliance. Which one would you∑they didn't, did they? No one says anything about it. And this is now nine years later believe me. They're still not mentioning oral appliances. No. Some are. Some sleep physicians are really good about this. But the majority still don't talk about this very often which is unfortunate because many of their patients are not doing well with CPAP machines just like you are. Out of given night, how many hours do you think you wear the CPAP machine? I find that I wake up with it all. Yeah. It tends to come off at sometimes. Sometimes people get up to go to the bathroom at 3 or 4 in the morning and then you just don't put it back on. I've done that too. I hear that story at a lot. Yeah, that's one of the things that I do a lot. Now I also noticed that your Epworth scale was 15. That's very sleepy. Anything over a 9 says that you're pretty sleepy. So that's another measure of the way we look at your fatigue levels. Also that you had some leg and limb movements. Now I will tell you that we'd like to treat the breathing first. And usually when we do, the limb movements go away. We think that the limb movements are largely in response to not breathing well and so we're moving our limbs. We're trying to get in a better position to breath. And we keep fighting that all night long and that's how we have more limb movements. So let's keep you breathing first and then the limb movements typically get better. I notice that your REM sleep has decreased. You only had 7% REM sleep and you should have 20%. Twenty percent of your sleep and this is regardless of age, 20%-25% of your night of sleep should be REM. Now that's dream sleep. You should be dreaming in REM sleep for a least 20% of the night. I can't remember the last time I had a dream. I hear that. In fact, usually when we treat patients one of the stories we hear when they come back in is I'm dreaming for the first time in years. I love hearing those stories. So you lose REM sleep and that's not good because REM sleep is important for life. REM sleep is so important they've tested removing REM sleep from horses and they lived about 2 weeks before they die. So we haven't tested humans yet. You'd probably a few who'd want to test. Anyway, we're not going to test humans. So we know that it's important for life. REM sleep is very important. And then I noticed you'd no slow wave delta sleep. This is your deep sleep. This is your deepest level of sleep that you really need as well and this is what we see with sleep apneic is the first stage of sleep they lose is slow wave sleep. I miss it. You're not getting any. I crave to have a good deep sleep. Yeah. When you get deep sleep, there are reasons for deep sleep too. First of al it's going to help improve your fatigue. But deep sleep is also important for memory, declarative memory names and numbers and things like that. That's very important. Also for regulation of two hormones that we'd talked about. They're Leptin and Ghrelin. Now Leptin and Ghrelin are regulated in deep sleep to the proper level. If you don't get deep sleep, these aren't regulated properly. Leptin tells you that you're full. Ghrelin tells you that you're hungry. During deep sleep, well if you don't get it, Leptin decreases Ghrelin increases and you just keep eating. So we know that sleep apnea causes, I'm sorry we know obesity causes more sleep apnea but we also know that once you have sleep apnea you continue to gain weight. So it just keeps going. So it's important to get this treated so that you can lose weight easier. You can improve your memory, improve your fatigue, all of these things. Then if you can't wear the CPAP, if it's something that you're, we called it intolerant to CPAP then what's when we're going to talk about oral appliance. Now there are three ways to treat sleep apnea. You've got CPAP which you've tried which you don't like. Oral appliances, which is the next step. If you're severe then we like you to try CPAP first and then you try oral appliances. If for some reason you can't and I have a feeling looking at this study that you'll do well with oral appliances and I'll talk to you about in some details in a minute but if you can't tolerate oral appliances then surgery. I'm not a big fan of surgery. And the American Academy of Sleep Medicine says oral appliance is better for your level anyway. So we're going to talk more about the reasons why an oral appliance would be effective for you. So I'm looking at the difference between like overall your AHI that means the number of times you stop breathing per hour and that you stop breathing for 10 seconds. So you have these 10 second, at least 10 second pauses where you're not breathing. That's what Tony was hearing. Okay. Or not hearing. He wasn't hearing any breathing. So that's an event. Okay. You have 26 of those events per hour. Wow. That's when you average all night long. Now when you rollover on your back and you go into REM sleep which is your paralyze sleep, your dream sleep, it gets much worst. It goes up to 78 from 26 all night up to 78. So more than once a minute you stop breathing for at least 10 seconds during that stage. The reason its worst during REM dream sleep is that we're paralyze for a very good reason. You don't want to act out your dreams. That's bad. If you can think of some dreams you've had in the past some of them you shouldn't be acting out. That's why we're paralyzed. And when we're paralyzed we can't move our jaw around and take a breath. The only things that move were our eyes. That's why they called it rapid eye movement. Our eyes are fluttering and our diaphragm to help us breathe. That's it. The only two muscles. So you're paralyzed in REM. You're on your back, worst case scenario and during that time 78 times per hour. But you know that tells us that an oral appliance will work will with you because we know that gravity is the problem. When you're on your side or on your stomach it's not very bad. But when you rollover on your back it gets way worst. That's because gravity is acting against you and it's pulling back and closing your airway off. Well these appliances that we make for your prevent that and they keep gravity from acting against you and closing your airway. So that's why I think looking at these numbers I think that you will be a good candidate. Now it's hard to guarantee anything. This is a medical procedure. All we can do is treat you and hope for the best. But we use these adjustable appliances. Now these are adjustable titratable we called it. So that we give you an appliance at a certain position where we're kind of guessing what would be a good position and then over time you adjust yourself further and further forward. And you're looking for silence and lack of fatigue, those two things. Tony can tell you if you're not snoring anymore. And then you judge your own fatigue levels how you feel in the morning when you wake up. So that's kind of how we judge, you judge at home. Then at some point, we follow you up with the sleep study. Now we have home sleep study unit that we will give you that you can do in the comfort of your own bed to see if the appliance is working. If it's not working well enough, we have you adjusting it further and further so until we get to that sweet spot. We will get you in for a followup study after you get the appliance done to make sure it is working like I said. And at that point, we send you back for another study and hopefully everything is good. Okay. Now there are some side effects we need to discuss. It's important that you discuss side effects with your patients because you want to cover the objection before it's an objection. You tell them for example that the teeth can get sore. Then when they come back and the teeth are sore, they say yeah you told me that. If you tell them you may increase your saliva. You may drool a little bit. They're not going to be surprised. They come back in and say, yeah I was drooling some. If you tell them your bite may change. And that's something that's very important because anytime somebody has an appliance with the jaw in a protruded position they live that way all night long they get up in the morning, what I'm going to tell you is that when you have an appliance you get in the morning and you go that's kind of weird. My bite will not go back. Now we're going to teach you some techniques for getting your bite back into the correct position. But even if you follow all of our directions, you could still have a bite change. Now I happened to think that that's a better position for you. That if your bite wants to live in a little bit further position that's going be better for you all around. Because during the day you can draw breath easier and it's a better what we called physiological position for you jaw. So it's sort of helping us get you in the right position. Your bite may feel a little bit funny and I've been doing this for 15 years. I have not had one patient that said Dr. Smith I can't live with this new bite. You got to get me back like you were. Because they're breathing better, they're feeling better, they're sleeping with their husbands again. All that stuff. It's good stuff. So they don't mind if their bite changes. But it's very important that you discuss bite changes with your patients because in about a third of our patient there is some measure of bite change. Sometimes it's very minor, sometimes it's macroscopic. So you got to tell them ahead of time. So that's about it. You can get a bite change. You can drool a little bit. Your teeth can get a bit sore. You might pop a crown off or something. Do you have any crown in your mouth? No. Okay so you will not pop any crown. That's a pretty rare thing but if it's tight on your teeth and you take it out every time in the morning there's always a chance pulling off a crown. So that's why we have to discuss that. So do you see any reason why you wouldn't want to go forward with treatments seeing that you can't wear a CPAP? Does it sound like something you'd like to do? Without a doubt. All right. When can we start? Well I can have April come in and she can get some impression. She's going to do a little bite registration on you too to find out where we want to start it out and then in about 4 weeks the appliance will be ready. We'll get you back in here and fit the appliance and we'll go from there. I am looking forward to it. All right. Well I'm so glad you came in to get this done today, Kelly, because I think we're going to give you a better life, better sleep. You're going to be a lot more sexy to Tony. Oh yeah. And I think overall you're going to be glad you came in. Other things I'm looking forward to by having this appliance is to be able to drive to work without being sleepy. Being able to be in the meeting and not be sleepy and to be at home and sleep quietly and not wake up the whole family for them to know I'm sleeping. I just want to have a good quality of life. There's nothing like having a really good deep sleep and I miss that, really one of the main things I want. I also want to have, I believe that by controlling my sleep and having that corrected using that appliance I believe that it will help me also with my weight. Because a lot of times I want to eat cause I'm tired, so I constantly put things in my mouth that maybe I shouldn't. So I think that would also help control my weight and my diet. It would help me focus because a lot of times my focus is off because I'm so tired and druggy. I believe that appliance will do just that.
|
 Submitting...
Submitting...


 FAGD/MAGD Credit Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement 7/31/2018 to 7/31/2021 Provider ID# 317928
FAGD/MAGD Credit Approval does not imply acceptance by a state or provincial board of dentistry or AGD endorsement 7/31/2018 to 7/31/2021 Provider ID# 317928